Clinical trials are a process in the healthcare world that has been happening for a long time. They play an integral role in not only finding new drugs and treatments for patients but also making sure that such medical solutions are safe and have the intended effect.
Clinical trials stand as a vital component in drug development. Preclinical testing may provide preliminary insights into a potential compound, but it is in the realm of clinical research that a drug’s safety and efficacy are rigorously assessed through its interaction with the human body.
As of early 2021, the tally of registered clinical studies surpassed 365 thousand, underscoring the magnitude of these investigations in advancing medical knowledge and therapeutic innovations.
The development costs of the average medication in the US range around $2.6 billion (2). The high costs for drug development mean that making sure the end result is safe to use and works properly is a definite must. That’s where clinical trials come in.
Understanding the phases of clinical trials is so important because it allows us to better understand the processes that come into play when creating a new drug.
This article will talk about the four different phases involved in clinical trials, what types of clinical trials are conducted in the medical industry, and what sort of regulations facilitate Food and Drug Administration (FDA) approval.
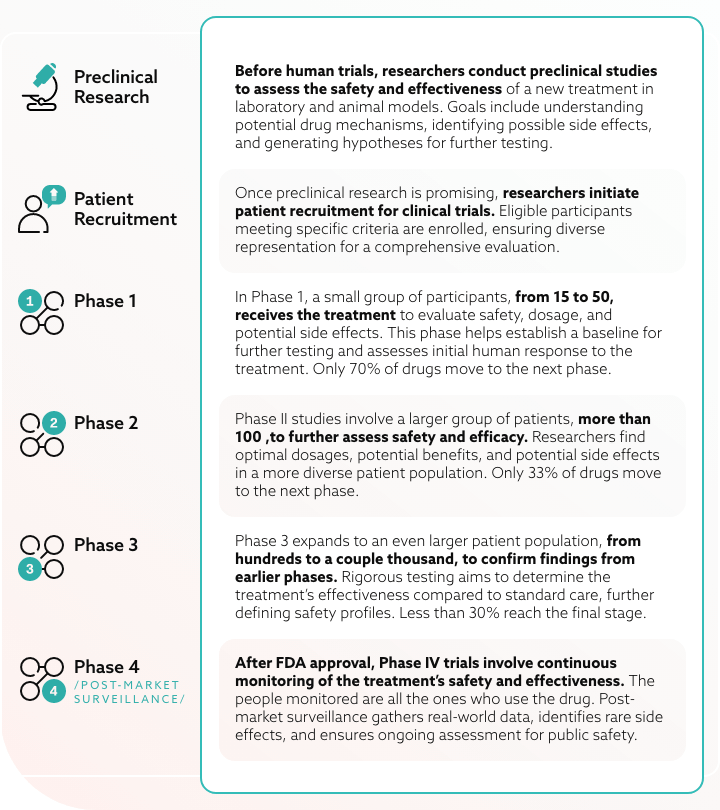
Preclinical research and initial study design
Preclinical research encompasses two fundamental categories: hypothesis-generating (exploratory) and hypothesis-testing (confirmatory) studies.
Hypothesis-generating endeavors are driven by scientific curiosity, intuition, and innovation, aiming to propose theories on disease pathophysiology and potential drug targets. Preserving the freedom of research staff in these exploratory pursuits is crucial for the vitality of preclinical science.
However, to validate hypotheses and justify clinical development, hypothesis testing laboratory studies are imperative. These studies, designed to demonstrate reproducible intervention effects in relevant animal models, demand the highest levels of rigor and transparency.
Clinical research teams create clinical trials to address specific inquiries related to a medical product. These trials adhere to a meticulously structured study plan, known as a protocol, which is devised by the researcher or the product manufacturer.
Before initiating a clinical trial, researchers analyze existing information about the drug to formulate research questions and objectives. Subsequently, key decisions are made, encompassing the selection of study participants, the study’s scale, duration, the inclusion of a control group, and strategies to minimize research bias.
Researchers also determine the drug administration methods, dosages, assessment protocols, and data collection procedures. The entire process spans various clinical trials’ phases, progressing from early, smaller-scale Phase 1 studies to more extensive, late-stage Phase 3 studies.
Regulatory agencies
There are two main regulatory bodies that need to be mentioned when talking about clinical trials. Those are the FDA and the European Medicines Agency (EMA).
Food and Drug Administration (FDA)
The FDA plays a crucial role in overseeing clinical trials in the United States, emphasizing patient safety, data integrity, and ethical standards.
Sponsors must submit an Investigational New Drug (IND) application before commencing trials, detailing the drug, study protocol, and participant safeguards. The FDA rigorously regulates clinical trials through all phases, collaborating with sponsors to uphold stringent scientific and ethical standards.
Adherence to Good Clinical Practice (GCP) guidelines is paramount, ensuring the reliability and validity of clinical trial data.
European Medicines Agency (EMA)
The EMA is a central regulatory authority overseeing clinical trials in EU member states, prioritizing patient safety, data reliability, and ethical standards.
Sponsors planning EU trials must secure Clinical Trial Authorization (CTA) from national authorities, with the EMA facilitating a streamlined process for specific multinational trials. The EMA collaborates with national authorities to enforce rigorous scientific and ethical standards across all clinical trial phases, from preclinical research to Phase 4.
Guided by GCP principles, the EMA ensures trials adhere to comprehensive guidelines, maintaining the integrity of trial data throughout the regulatory process.
Patient recruitment and informed consent
Patient recruitment involves the identification and enrollment of eligible human volunteers into the trial. This process often begins with healthcare professionals identifying potential clinical trial participants based on specific criteria outlined in the trial protocol.
Recruitment strategies may include outreach through medical facilities, community hospitals, events, or online platforms. Different treatment groups may vary but research studies seek to have treatment groups with diverse populations to offer a greater sample of how a new treatment affects different people.
The informed consent process is a cornerstone of ethical clinical research, emphasizing transparency and participant autonomy. Before joining a trial, individuals must be provided with detailed information about the current treatment’s purpose, procedures, potential risks and long-term benefits, and their rights as participants.
This information is presented in an informed consent document, and participants are given the opportunity to ask questions and fully understand the implications of their involvement. The decision to participate is voluntary, and participants have the right to withdraw at any time without facing negative consequences.
Each clinical trial has specific prerequisites, referred to as eligibility criteria, which must be satisfied for participation. Research team members usually look at things like age, risk factors, medical background, health status, and genetic changes in the tumor in cancer clinical trials for example.
These criteria serve to minimize medical variations among participants, mitigate the potential for harm, and restrict the trial to individuals most likely to derive benefits. By ensuring participants share certain characteristics, researchers can enhance the confidence in attributing results to the tested intervention or drug rather than extraneous factors.
Types of clinical trials
Clinical trials encompass a variety of types, each serving specific purposes in advancing medical knowledge and improving patient outcomes:
- Treatment Trials are a common category, typically spanning Phases 1, 2, and 3. They aim to assess the effectiveness and safety of new treatments, medications, or interventions. Participants in these trials are individuals with the targeted health condition.
- Prevention Trials can involve Phases 2 and 3. These trials evaluate interventions designed to prevent the development or recurrence of a health condition. Participants in prevention trials are individuals at risk but without the specific condition.
- Diagnostic Trials primarily operate in Phases 2 and 3, focusing on developing and refining tests or procedures for diagnosing medical conditions. Participants are usually individuals suspected of having the specific condition.
- Screening Trials, concentrated in Phases 2 and 3, assess the effectiveness of screening methods for early detection of diseases. Typically, these trials involve individuals without symptoms.
- Quality of Life Trials aim to improve the comfort and quality of life for individuals with chronic illnesses which may span Phases 2 and 3. Participants in these trials are individuals with the targeted chronic condition.
- Observational Trials are not clinical trials but observational studies. They involve observing participants in their natural settings without intervening. Participants may have a specific health condition or be healthy individuals.
Finally, Expanded Access (Compassionate Use) Trials vary in phase, providing access to experimental treatments for patients with serious or life-threatening conditions who don’t qualify for standard clinical trials.
The phases of clinical trials explained
Below, we will explain the purpose and elements of each clinical trial phase.
Phase 1 clinical trials: Safety and dosage
The primary objectives of Phase I trials are to assess the safety of a new treatment, determine the optimal administration method, and evaluate the treatment’s efficacy.
This phase typically involves 15 to 50 patients in small groups, also called cohorts. In it, each group receives different doses of the new drug. Initial cohorts receive a starting dose, and subsequent treatment groups receive escalated doses.
Monitoring for severe side effects is a crucial aspect. If no severe side effects are observed in a cohort, the next treatment group receives a higher dose until the optimal dosage is identified. Successful and safe treatments progress to Phase II trials for further study.
Following Phase 1, the outcomes are gathered, assessed, and submitted to the FDA for approval to advance to Phase II clinical trials. In the event that the findings reveal that the treatment is linked to one or more severe adverse events, the FDA may withhold permission for progression to Phase 2.
On average, 70% of drugs move on to the next stage.
Occasionally, a treatment initially approved for one disease may be explored for treating another ailment. This is known as repurposing a drug, and it can potentially expedite the clinical trial process. It allows for swifter progression into Phase 2 clinical trials since the safety profile established in the Phase 1 trial has already been examined.
Phase 2 clinical trials: efficacy and side effects
The objective of a Phase II clinical trial is to determine the appropriate dosage and effectiveness in treating a specific disease.
This phase typically involves a larger number of volunteers with the disease, usually no more than 100 patients. The trial sponsor may employ various methods, often assigning participants to different treatment groups, each receiving varying doses or methods of treatment.
Usually, there is a control group receiving either the standard treatment or a “placebo” which is like a sugar pill or inert injection that mimics the real drug, but has no effect on the patient.
Patient groups receiving different treatments are compared to the control groups. If the Phase II trial results indicate that the treatment did not outperform the existing standard of care, or led to disease acceleration or unexpected serious adverse events, the FDA may withhold permission for Phase III trials. In such cases, further testing of that treatment is usually halted, removing it from consideration for market approval.
According to the FDA, no more than 33% of drugs move on to later phase trials.
Phase 3 clinical trials: large-scale testing
Phase III clinical trials involve a significantly larger group of volunteers from hundreds to thousands and primarily aims to assess the safety and effectiveness of the treatment across diverse individuals.
The plan typically includes assigning participants to treatment or control groups, with the possibility of treatment combination of drugs or different components. Again, there is a control group receiving either the current treatment or a placebo.
Following the Phase 3 clinical trials, the health outcomes of patients receiving different treatments are compared to control groups. If the results indicate that the treatment did not surpass the existing treatments or caused disease acceleration or unexpected serious adverse events, the FDA may withhold permission to proceed to submit a New Drug Application (NDA).
This special NDA encompasses all discoveries from Basic Research/Drug Discovery to Phase 3 clinical trials and is submitted to the FDA for approval to sell the treatment on the market.
It is important to mention that Phase III studies are most often double-blind studies, which means that neither you nor the researchers know who is receiving the placebo and who the new treatment is. Whether you get the real drug or not is randomly assigned by a computer.
Unlike the other two phases which take from a couple of months to two years, a Phase III trial takes from one to four years.
Less than a third of the drugs reach the final stage.
Phase 4 clinical trials: regulatory approval and post-marketing surveillance
Following FDA approval and large-scale drug manufacturing by the sponsor, the process enters Phase IV clinical trials – post-market surveillance.
Throughout the treatment’s market presence, the FDA diligently monitors public safety and potential adverse events. This phase usually includes all the people who use the drug – thousands or tens of thousands.
Additionally, mandatory or optional Phase 4 post-marketing clinical trials may be conducted. They aim to gather more data on risks, benefits, and long-term effects, or test the product in specific patient populations. The FDA offers extensive information on all drugs currently available in the U.S. market.
The future of clinical trial methodologies holds a lot of potential given the development of newer and better health technologies for disease detection and genetic analysis.
Adhering to standard practices when it comes to clinical research is integral to maintaining a steady grasp on the evolution of drug development procedures. The best way to ensure safety and efficiency with new treatments is to not forget the practices and phases that brought us here.

Whether you’re a startup, a Fortune 100 company or a government organisation, our team can deliver a solution that works for you.
BGO Software