Imagine a world where each decision about health is based on firm scientific proof—a world in which patients will receive optimum treatments that help keep treatment costs as low as possible.
From the lighting-fast developments with COVID-19 vaccines to state-of-the-art medical devices and new surgical procedures, health technology assessment (HTA) gives shape to the future of healthcare.
Yes, but what is HTA, and why is it so important in today’s medical environment?
In this article we show the intriguing world of HTA: its origination, methodologies, and real-world applications. We’ll see how it influences health policies and healthcare practices across the world and analyze its role in ensuring newer technologies truly add value to both patients and health systems.
Introduction to Health Technology Assessment (HTA): Importance and scope
HTA is a mechanism to guarantee that health technologies are safe, effective, and offer value for money. This ensures that resources are efficiently utilized and technologies are deployed in ways most capable of benefiting health in the context of ethics and society.
The scope of HTA extends to the evaluation of such technologies at different stages of their life cycle—from development and introduction to widespread use and eventual obsolescence.
In the US, the Congressional Budget Office concluded that “roughly half of the increase in healthcare spending during the past several decades was associated with the expanded capabilities of medicine brought about by technological advances”. (1)
The multidisciplinary process
In the world of Health Technology Assessment (HTA), the magic happens when diverse minds unite.
Imagine a team in which doctors bring clinical insight, economists bring cost-effectiveness modeling, policymakers bring regulatory compliance, and patients bring forward the needs and experiences voiced.
It generally encompasses the following basic steps:
- Тhe selection and prioritization of health technologies for assessment;
- Gathering and analyzing data on the safety, efficacy, and cost-effectiveness of these technologies;
- Аssessment of broader social, ethical, and economic implications. Synthesize the evidence to inform policy decisions and clinical guidelines.
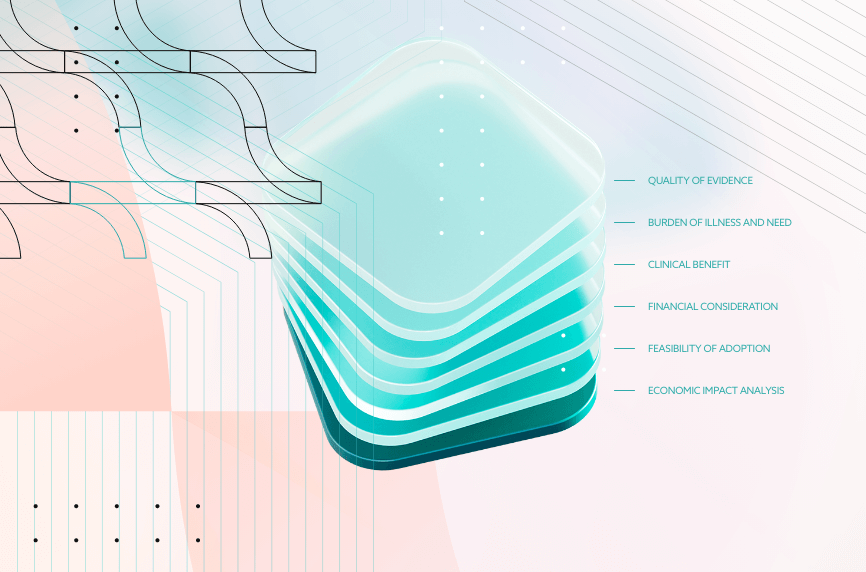
Evidence-based decision making in HTA: factors and methods

This process safeguards patient care, making sure that the best, most effective treatments are available to those who need them in the health care system.
HTA uses different explicit methods for making decisions in a systematic manner. More about them is described in the paragraphs below.
Quality of evidence
The goal of the HTA and systematic review is to obtain a more accurate estimate of the treatment effect. The reason is that high-quality evidence is essential to justify health care spending on new technologies.
Some key elements are:
- Methodological quality: Do critical appraisal checklists for observational, descriptive, RCT, systematic review, and observational studies get used when evaluating the quality of evidence for individual studies? Have studies with poor methodology still been left out of this analysis?
- Hierarchy of study designs: The risk of bias and the ways in which health research designs prevent it, determine the degree of evidence. Also, a level of evidence will be assigned to each type of evidence in order to estimate the review findings’ credibility.
- Grades of recommendation: Think about whether the positive effects outweigh the negative ones and whether there is sufficient high-quality evidence to back up its application.
Also consider whether the use of resources is positively impacted or not, and whether consideration was given to values, preferences, and the experience of the patient.
Burden of illness and need
This part analyzes what is the burden of illness that the target condition, for which the technology is being used, has on society. This takes into account factors such as incidence, prevalence, years of life lost, years lived with disability, and years of life adjusted for disability.
Then, it’s important to assess what is the degree to which technology is required to manage the target condition in comparison to the availability of alternatives.
Clinical benefit
The clinical benefit simply refers to the positive impact that a technology or treatment has on health and well-being.
Elements include:
- Safety: The frequency and severity of unfavorable events related to the technology, as well as a comparison with the alternatives that are available.
- Effectiveness: Technology’s effectiveness, including a comparison with other options. It may be assessed using a variety of metrics, including mortality, survival, morbidity, length of stay, and odds ratios. It is important to take into account the scope and direction of the technology’s impact.
- Suitability of patient selection: Is the proposed patient selection group appropriate?
Needless to say, ensuring clinical benefits is crucial for maintaining a high quality health system that is able to promote health the right way.
Financial consideration
When considering the adoption of new health technology, health technology assessments are crucial to ensure economic feasibility and value for money. This involves analyzing the costs, potential funding implications, and the overall budget impact to make informed decisions.
Here, there are two fundamental elements: the price of health technology and its cost-effectiveness.
The price of health technology regards the system and/or device cost, as well as the total estimated cost of the device for the local health network and the number of patients stated annually.
Cost-effectiveness, on the other hand, is about the net budget impact of the new technology in terms of economic feasibility.
Here, various factors play a role, including:
- Work-up costs;
- Hospitalization costs;
- Expenses for other system enablers such as IT, capital projects, workforce compensation, hiring, and training;
- Funding implications such as statewide or superspecialty status impacted by downstream costs;
A cost-effectiveness analysis examines how much a technology costs in relation to its effects on health.
It is possible to apply experience from foreign or different jurisdictions.
Feasibility of adoption
Implementing new health care technology requires careful consideration of various factors to ensure its success.
This analysis aims to provide a comprehensive overview of the key elements involved in assessing the feasibility of such initiatives:
- Organizational feasibility: The degree to which health technology can be implemented smoothly by examining additional barriers and/or enablers. This depends on infrastructure, location, clinical services capability framework, impact on other service streams (like rehabilitation services), and the applicant’s capacity to conduct field evaluations (where applicable).
- Credentialing and competency: Accreditation of suitable medical professionals, including upon course completion or training
Factors that indicate technological proficiency and experience, such as quantity of operations to be performed under supervision or the annual or service-specific cases.
Economic and societal impact analysis in HTA

Economic evaluation forms a core component of health technology assessment as it provides a structured method for comparing technology cost and consequences within the health system.
Principal types of economic evaluations in the course of HTA include:
- Cost-of-illness analysis: These estimate the impact of a disabling condition on a specific population, typically within a defined region or country. Different costs arise from the direct treatment and the indirect lost productivity.
- Cost-minimization analysis: This is used when two or more different interventions are being compared as equivalent in terms of outcomes, having been evaluated comprehensively. It identifies the least costly of the options under review.
- Cost-effectiveness analysis: Compares costs in monetary units of different interventions with their impacts in natural units, such as life years gained or cases detected. CEA is approachable for examining the most efficient way of getting a particular health outcome.
- Cost-utility analysis (CUA): a type of CEA, which uses an outcome measure known as a quality-adjusted life year (QALY). This allows the comparison of different interventions with different health effects.
- Cost-Benefit Analysis (CBA): Compares monetary quantified costs and benefits, as finally measured. This method is applied to find out whether the benefits of a certain intervention actually justify its costs.
- Budget-Impact Analysis (BIA): Provides an examination of the impact that going for a new health technology will have on the finances drawn under a defined contextual exception, say, to a particular budget within a healthcare provider’s budget for the year.
Case Studies and Examples Case studies can be used to give practical real-life examples for the application of economic and societal impact in HTA.
For example:
- Basic childhood vaccines : The high cost-effectiveness of basic childhood vaccines illustrates the very low cost per DALY gained in improving population health.
- Tuberculosis treatment: There can be remarkable health economics in this treatment by directly observed treatment short course (DOTS) tuberculosis that is cost-effective from the view of many cost-saving and health benefits, particularly in countries of low and medium incomes.
- Coronary Artery Bypass Grafting (CABG): This high-cost intervention is cost-effective for specific patient groups by improving life expectancy and quality of life.
Taking these into account can greatly improve the health care decision-making process and provide policy-makers with actionable insights for improving health services.
Patient-centered approaches in HTA
Patient perspectives play a pivotal role within HTA by offering insight into the real-world nature of health technology impacts, ensuring that the process remains patient-focused.
Patient focus ensures that decisions to deliver healthcare are made taking into consideration what matters most to patients, like the quality of life and the status of function at the time.

Deliver a world-class Healthcare project–with high-skilled, seamlessly integrated IT talent
Learn how from our consultants. We work with clients worldwide.
Methods to integrate patient input
Patient feedback helps improve current health technologies by providing insights of their impact on quality of life. This information guides healthcare providers and decision-makers in improving technologies to better meet patient needs.
Feedback can be collected through:
- Surveys and questionnaires: Devices to collect a patient’s experience and satisfaction include PPPC and CCM (Patient Perceived Problem Checklist and Care Coordination Measure).
- Patient involvement: The patients are involved in HTA processes, and they basically participate in giving inputs and reviewing the reports.
- Patient-reported outcomes (PROs): Outcomes reported by patients on their own health status and quality of life, typically through direct measurement within studies.
- Focus groups and interviews: This is when patients are included in discussing their experience with health technologies.
Gathering feedback can inform decision making in both the medical equipment area and other health technologies needed for modern personalized medicine.
Regulatory and reimbursement aspects of HTA

Regulatory procedures in Health Technology Assessment ensure that before a health technology is available in the market, its safety and efficacy are guaranteed.
This is managed by independent regulatory agencies like the FDA in the US and EMA in Europe. They lay down guidelines for post-market surveillance so that the tracking of performance and safety issues continues beyond market launch.
Role of HTA in reimbursement decisions
HTA findings are used by payers to make informed decisions on which technologies to cover, how pricing should be set, and under what conditions technologies must be reimbursed.
Examples of regulatory and reimbursement frameworks include:
- Coverage with evidence development (CED): A managed entry scheme whereby new technologies are covered while additional evidence is collected to confirm their effectiveness and safety.
- Performance-linked reimbursement: A reimbursement arrangement where the level of return is directly linked to the realization of some given health outcomes, that has technologies attain expected benefits in real-world use.
- Conditional treatment continuation: Payment is made as long as patients are meeting predefined treatment goals, such as clinical improvements or biomarker targets.
Ethical considerations in HTA
Balancing ethical issues related to cost and effectiveness is based on the evaluation not only of clinical and economic benefits accruing from health technologies, but also with respect to their ethical dimensions.
For instance, as much as technology would be cost-effective, it must also be with respect to ethics. This is to ensure no particular group is put at a disadvantage and that overall health and well-being are promoted fairly.
There are several ethical issues that have to be dealt with in HTA like the value placed on human life and the broader socioeconomic and legal dimensions:
- Resource Allocation: The determination of the allocation of insufficient healthcare resources ethically so that all patients have equal access to upcoming technologies.
- Informed Consent: A patient adequately makes an informed decision regarding the balance of benefits against risks offered by a health technology, where his or her consent is elicited prior to the use of that particular technology.
- End-of-life care: This is the balancing act between advanced technologies to extend life and ethical considerations of quality of life together with patient autonomy.

Implement robust methodologies for decision making in HTA
Use systematic methods to evaluate health technologies, considering clinical benefit and cost-effectiveness.

Methodological frameworks in HTA
HTA utilizes various methodological frameworks to ensure robust evaluations:
PICO/PICOTS
PICO/PICOTS stands for Population, Intervention, Comparator, Outcome, Timing, Study design.
This framework is used to structure research questions and ensure that all critical elements are considered.
Analytic frameworks
Also known as causal pathways, these depict direct and indirect relationships between interventions and patient outcomes.
They help in defining key questions and identifying important relationships where evidence might be lacking.
Integrative methods
Include systematic reviews and meta-analyses, which combine data from multiple studies to provide a comprehensive summary of the evidence.
Below, you can see the strengths and limitations of alternative methodologies:
|
Strengths |
Limitations |
|
|
Systematic reviews and meta-Analyses |
Good summaries, reduce bias |
Limited by quality of primary studies |
|
Randomized Controlled Trials (RCTs) |
High internal validity |
Expensive, time-consuming |
|
Decision-analytic Models |
Simulation of situations |
At the mercy of data quality |
International collaborations and harmonization in HTA
Such international collaborations in Health Technology Assessment increases the effectiveness of assessments through resource sharing, expertise, and information sharing. This collaboration aids HTA agencies in going beyond the constraints of any single assessment through collective knowledge and capabilities.
Standardized methodologies and good practices are promoted at the core, which are characteristic of sustaining quality in different countries.
Harmonization efforts across countries
Harmonization in HTA activities means aligning assessment methodologies and processes across countries to ensure consistency and comparability of results.
This would be attained through international networks such as EUnetHTA, which provides a framework for collaborative HTA projects between member states. By this way, it succeeds in capturing contextual factors—precisely, different healthcare systems and regulatory environments—that make the HTA findings relevant and applicable across various settings.
Below, you can see some of the best examples of successful international collaborations.
EUnetHTA core model
EUnetHTA has elaborated a core model setting a common basis for conducting these HTAs in a collaborative way.
It covers several domains, among them the clinical effectiveness domain, the economic evaluation domain, and the ethical analysis domain.
International network of agencies for Health Technology Assessment
INAHTA offers a network whereby governmental or quasi-governmental HTA agencies across the world collaborate and intercommunicate.
Bringing together, at a single platform, such expertise therefore obviously reinforces the quality as well as efficiency of HTAs by encouraging knowledge and best practice exchanges between them.
Cochrane Collaboration
This should, therefore, be accompanied by systematic reviews of healthcare interventions which the Cochrane Collaboration is to undertake.
That unites experts from more than 100 countries in a decentralized model, gives support to harmonization efforts in HTA methods and improves the global evidence base for healthcare decision-making.
In conclusion, future HTA will be marked by adaptability to new challenges, innovation in the methods used, and more use of its evidence for policies and practices all over the world. Remaining at the leading edge of advancements and maintaining a patient-centered view, HTA will continue to ensure health gains and the sustainability of health systems well into the future.
SourcesTechnological Change and the Growth of Health Care Spending
Types of Economic Evaluation
Health Technology Assessment (HTA) Decision Summary
Introduction To Health Technology Assessment