In the realm of modern healthcare, personalized medicine emerges as a groundbreaking approach, heralding a new era in the way medical care is delivered and experienced.
This innovative paradigm shifts away from the traditional ‘one-size-fits-all’ methodology. Instead, it embraces a more tailored approach where treatments and preventive strategies are finely tuned to individual patient characteristics. At its core, personalized medicine is a confluence of genetic understanding, technological advancements, and sophisticated data analysis. They all converge to offer care that is as unique as the patient receiving it.
In this article, our objective is to delve into the intricate world of personalized medicine, unraveling its core principles and understanding how it transforms the landscape of medical treatment and disease prevention
Understanding personalized medicine
Personalized medicine, also known as precision medicine, represents a paradigm shift in healthcare.
It’s a medical model that categorizes individuals into distinct groups, with medical decisions and treatments tailored to the individual patient based on their predicted response or risk of disease. This approach contrasts with traditional methods where a ‘one-size-fits-all’ strategy is often employed
Historical evolution
The concept of tailoring treatment to patients can be traced back to Hippocrates. Doctors have always considered a personalized approach to each patient to be of great value.
However, the term “personalized medicine” has gained prominence recently due to advancements in diagnostic and informatics approaches, particularly in genomics and genome biology. They provide a solid foundation for grouping patients based on their molecular disease profiles.
Key principles
The two key principles of personalized medicine are as follows:
- Individualization: Personalized medicine advocates for treatments based on a person’s genetic makeup, considering the unique variations in their genome. This personalized method acknowledges that while most genetic variations do not influence well-being, they can greatly affect an individual’s health when combined with environmental factors and lifestyle behaviors.
- Precision: Utilizing advanced technologies, such as genome sequencing, personalized medicine can identify specific DNA mutations that are linked to diseases. This enables more precise diagnosis and treatment targeted at these specific mutations.
These principles combined greatly reduce the trial and error inefficiencies, allowing healthcare professionals to better understand disease and address it.
Contrast with traditional medicine
Precision medicine improves patient results in two main ways, differentiating it from traditional medicine:
- Customization vs. one-size-fits-all. Traditional medicine often follows a generalized approach, whereas personalized medicine customizes healthcare to subgroups of patients based on genetic and molecular characteristics.
- Predictive and preventive. Unlike traditional methods, personalized medicine aims to predict susceptibility to diseases and tailor preventive strategies, moving away from reactive treatments.
Else said, this approach changes the emphasis from reaction to prevention when it comes to the routine practice in healthcare.
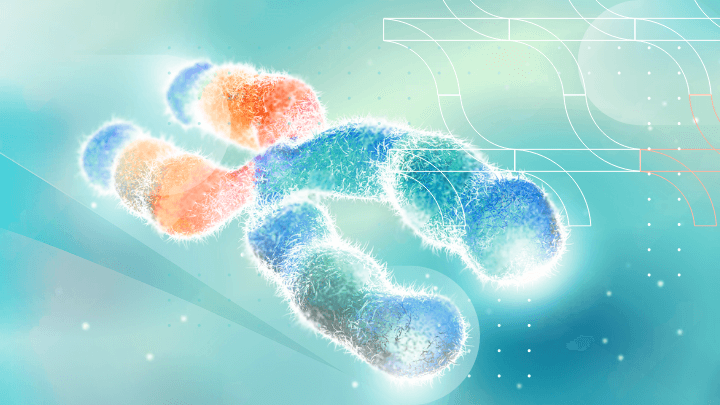
The role of genetics in personalized medicine
Genetic foundations: understanding variability and health implications
Genetic variability is a fundamental aspect of human biology. Each individual possesses a unique variation of the human genome, which contributes significantly to their health and response to treatments.
Although many genetic variants do not impact health, certain variations can greatly influence individual health outcomes. This variability is intertwined with other factors like environment and behaviors, shaping overall health profiles.
Modern personalized medicine leverages technologies such as DNA and RNA sequencing to uncover these genetic variations. These methods reveal mutations and gene expressions that are directly linked to diseases ranging from cystic fibrosis to cancer.
Genetic information guiding treatment
Genotyping, the process of determining an individual’s DNA sequence using, for example, next-generation sequencing (NGS tests) plays a crucial role in personalized medicine.
By comparing a patient’s genome to reference genomes, healthcare professionals can identify a genetic variation responsible for diseases. This detailed genetic information allows for more accurate diagnoses and tailored treatment plans.
This method is key for drugs with varying effectiveness and side effects across individuals and will become increasingly important in future clinical pharmacology. Picking the right drug and the right dose will increasingly rely on genetic analysis as therapies become more specialized to different mutations.

Explore the Future of Healthcare with Personalized Medicine
Discover how software is driving unprecedented personalization in medicine.

Ethical considerations: patient privacy and discrimination in genetic data
The increasing use of genetic information in healthcare raises critical ethical concerns, particularly regarding privacy and potential discrimination.
As genetic testing becomes more prevalent, ensuring the confidentiality and security of genetic data is paramount. There is also the risk of genetic discrimination in areas such as employment and insurance. Balancing the benefits of personalized medicine with these ethical challenges is vital for the responsible advancement of healthcare practices.
As we have mentioned, pharmacogenomics is a crucial aspect of personalized medicine, so it is worth taking a closer look at its principles and contribution to modern treatments.
Pharmacogenomics and personalized medicine
Definition and significance in drug therapy
Pharmacogenomics is a branch of personalized medicine that involves tailoring drug treatment to an individual’s genetic makeup. This approach significantly enhances the effectiveness of drug therapy by ensuring that medications are compatible with the patient’s genetic profile, thereby maximizing efficacy and minimizing adverse reactions.
Genetic profiling plays a crucial role in determining how an individual will respond to certain medications. By analyzing a person’s genetic composition, healthcare professionals can predict the efficacy and safety of various drugs, leading to more accurate and safer prescriptions.
This approach is instrumental in avoiding adverse drug reactions, which are often due to genetic variations affecting drug metabolism.
Examples of pharmacogenomics in clinical practice
Below, we will discuss some prominent examples of pharmacogenomics in the context of clinical practice.
Warfarin dosing
Warfarin, a commonly prescribed anticoagulant, shows considerable variability in its effectiveness and safety among different individuals. This variability is largely due to genetic differences in enzymes encoded by the CYP2C9 and VKORC1 genes.
Pharmacogenomic testing allows for the adjustment of warfarin doses based on these genetic factors, significantly reducing the risk of bleeding and enhancing therapeutic outcomes.
Companion diagnostics
Companion diagnostics are assays developed for specific drugs to determine their suitability for a particular patient. These tests incorporate pharmacogenomic data to guide prescribing decisions, ensuring that as many patients as possible receive medications that are most likely to be effective and least likely to cause adverse effects.
Clinical trial selection
Pharmacogenomic information is increasingly used in the context of pharmaceutical clinical trials. By understanding a patient’s genetic makeup, researchers can more accurately determine which individuals are likely to benefit from a specific treatment, thereby increasing the safety and effectiveness of clinical trials.
This approach also supports the development of therapies for smaller patient populations that may not respond to more general treatments.
Targeted cancer therapies
In cancer treatment, pharmacogenomics has led to more precise therapies. For example, the efficacy of Tamoxifen, a drug used in breast cancer, is influenced by genetic variations in the CYP2D6 gene. Pharmacogenomic testing can identify patients who are less likely to benefit from Tamoxifen, allowing for the selection of alternative treatments that are more likely to be effective.
Pharmacogenomics represents a significant advancement in personalized medicine, enabling health care providers to offer more targeted and effective treatments based on individual genetic tests.
Let us explore the world of targeted therapies further, especially in light of their recent contributions to improved cancer care.
Targeted therapies in personalized medicine
Targeted therapy represents a significant advancement in the field of personalized medicine, particularly in cancer treatment. Unlike traditional approaches, which often have a broad impact on the body, targeted therapies are designed based on deep molecular analysis to attack specific molecular changes in cancer cells.
These therapies work by blocking or turning off signals that promote cancer cell growth and division, preventing cells from living longer than normal, or directly destroying the cancer cells.
They can be divided into several types, including monoclonal antibodies and small-molecule drugs:
- Monoclonal antibodies: These block specific targets on or around cancer cells and can deliver toxic substances directly to them.
- Small-molecule drugs: They interfere with the processes that help cancer cells multiply and spread. For example, angiogenesis inhibitors starve tumors by preventing the formation of new blood vessels needed for tumor growth.
The choice of targeted therapy depends on the genetic, immunological, and proteomic profiling of the individual’s cancer.
Role in cancer treatment
The impact of targeted therapies on cancer care has been profound, particularly in the treatment of molecularly driven lung cancer. There, they have demonstrated superior activity and better toxicity profiles compared to traditional chemotherapy. These therapies require molecular testing for driver mutations, which significantly influence patient survival and quality of life.
For instance, in lung cancer, nearly 30% of cases may be driven by specific mutations, with targeted therapies showing dramatic improvements in outcomes. Similarly, in breast cancer, targeted therapies are used for HER2-positive cancers, which constitute about 20-25% of all breast cancers.
Chronic myeloid leukemia (CML) treatment has also been revolutionized with targeted therapies focusing on the BCR-ABL gene.

Empower Your Health Journeywith Personalized Medicine Software
Discover how it tailors medical approaches based on individual characteristics, optimizing treatment outcomes.
Broader applications
While most prominently used in cancer treatment, the potential of targeted therapies extends to other diseases as well. The principle of using genetic and molecular information to tailor treatments can be applied across various medical conditions, such as cardiovascular disease, autoimmune conditions, and even Alzheimer’s.
As we improve our understanding of disease and its genetic and molecular basis, we can expect to see targeted therapies making significant impacts in other areas of medicine as well.
Personalized medicine and data analytics
We have talked a lot about the various achievements of personalized medicine, but it is equally interesting and valuable to know what methods scientists employ to develop all these novel therapies.
A crucial ingredient in the recipe of personalized genomic medicine is the integration of various data types and the application of predictive analytics, although this also presents certain challenges.
Data integration
In personalized medicine, the integration of diverse data types is pivotal.
This includes:
- Genomic data: Information about a patient’s DNA. For example, identifying genetic markers linked to specific diseases can guide the selection of suitable medications.
- Clinical data: This encompasses personal medical and family history, laboratory test results, and current health status. For instance, a patient’s response to a previous treatment can inform future treatment plans.
- Environmental data: Includes lifestyle and environmental factors such as diet, exercise habits, and exposure to toxins. For example, understanding how a patient’s environment influences their health can lead to more effective treatment strategies.
The amalgamation of these data types through advanced analytical techniques enables healthcare providers to develop a comprehensive understanding of a patient’s health and tailor treatments accordingly.
Predictive analytics
Predictive analytics in personalized medicine involves using data analytics to forecast treatment outcomes.
Key applications include:
- Treatment optimization: By analyzing how similar patients have responded to various treatments, doctors can predict how a current patient might respond, thus selecting the most effective therapy.
- Risk assessment: Predictive models can identify patients at high disease risk, allowing for early intervention or preventive measures.
For example, if data analysis reveals that patients with a particular genetic makeup respond well to a certain cancer drug, doctors can prescribe that drug to similar patients, potentially improving treatment success rates.
Challenges
Despite its promise, the implementation of personalized medicine and data analytics faces several challenges:
- Data management. The sheer volume and complexity of data require sophisticated systems for storage, processing, and analysis.
- Privacy concerns. Handling sensitive patient data demands stringent measures to protect privacy and ensure data security.
- Ethical issues. Decisions regarding who gets access to personalized treatments and how these treatments are allocated raise ethical questions.
It is evident that personalized medicine is a complex undertaking requiring sophisticated and reliable tools in order to maximize the chances of success. This is why we now turn our attention to some of the “tools of the trade” and explore the types of software used in personalized medicine.
Personalized medicine software
Personalized medicine software is integral to the rapidly evolving technology landscape of healthcare, offering nuanced and individualized treatment approaches.
This section delves deeper into the intricacies of such software, providing a clearer understanding of its types, functionalities, integration with healthcare systems, and future development trends.
Types of software solutions in personalized healthcare
The variety of software in personalized medicine is vast, each type catering to specific needs in the healthcare continuum:
-
- Genomic analysis software: This software analyzes a patient’s genomic data to identify unique genetic markers. An example is software used in gene therapies and cell therapies, like CAR-T cell therapies for cancer treatment, where the software guides the customization of therapies based on the genetic profile of cancer cells and the patient’s immune system.
- AI-driven diagnostic and predictive tools: These tools leverage AI and big data for early disease detection and treatment planning. For instance, AI models in Oncora Medical’s patient care platform integrate EHRs and other clinical data to identify high-risk patients and optimize treatment plans.
- Clinical decision support systems (CDSS). CDSS use AI algorithms to analyze patient EHRs, aiding clinicians in making more informed decisions. They can, for example, predict the likelihood of patient readmission or complications post-surgery.
- Drug discovery and development platforms. These platforms use AI to expedite the drug discovery process, predicting the efficacy of drug candidates and identifying novel applications for existing drugs.
As a global resource for clinical use, personalized medicine software has the potential to reduce health care costs by focusing more on prevention and reducing the failure rate of disease treatment.
Functionality and features of personalized healthcare solutions
The core functionalities of personalized medicine software are sophisticated and multifaceted:
-
- Data integration and analysis. These systems integrate and analyze diverse data types, including genomic, phenotypic, and lifestyle data, to provide comprehensive insights into patient health.
- Predictive analytics and simulation. Leveraging machine learning algorithms, the software can simulate treatment outcomes and predict patient responses, aiding in the selection of more effective drugs and treatment plans.
- Real-time monitoring and adaptation. Advanced platforms enable real-time monitoring of patient responses, allowing for dynamic adjustment of treatment strategies.
Last but not least comes interoperability with existing systems. Key to their utility is their ability to seamlessly interface with existing healthcare databases and EHR systems.
Integration with healthcare systems
Successful integration is essential for the utility of personalized medicine software.
For this purpose, two processes are crucial:
- Data interoperability and sharing. It’s crucial that these systems can efficiently exchange data with other healthcare software while maintaining data integrity and security.
- Regulatory compliance. They must adhere to healthcare regulations, including data privacy laws and medical device standards.
Future trends
Looking ahead, the trajectory of personalized medicine software is marked by several promising developments:
- Enhanced AI and machine learning. Continued advancements in AI will lead to more sophisticated data processing capabilities and predictive accuracy.
- Wearable technology integration. Increasing use of wearable technology will feed more real-time data into personalized medicine applications, enhancing monitoring and treatment adjustment capabilities.
- Patient-centric approaches. There will be a greater emphasis on patient-specific data, including lifestyle and environmental factors, making treatments more personalized and effective.
Collaborative developments are also on the rise. We can expect more cross-disciplinary collaborations, bringing together medical professionals, data scientists, and software developers to innovate in the field of personalized medicine.
The bottom line
Personalized medicine is a beacon of innovation in healthcare. It promises a future where treatments are no longer dictated by a ‘one-size-fits-all’ approach but instead precisely tailored to individual patients.
This revolutionary concept focuses on the patient’s unique genetic, environmental, and lifestyle factors, aiming to optimize treatment efficacy, minimize adverse effects, and significantly improve patient outcomes.
The growing advancements in areas like genomics, artificial intelligence, and wearable technology integration are continuously propelling personalized medicine toward redefining our understanding of healthcare.
As the FDA continues to work on evolving privacy and safety guidelines and knowledge bases expand, active clinician input from institutions like the American College of Physicians will be instrumental in shaping the future of personalized medicine.

Whether you’re a startup, a Fortune 100 company or a government organisation, our team can deliver a solution that works for you.
BGO Software
By addressing these key areas and overcoming the associated challenges, personalized medicine stands to not only revolutionize medical practice but also to significantly enhance the quality of life for patients worldwide, marking a new era in healthcare.